Cervical cancer occurs when the cells of the cervix grow abnormally and invade other tissues and organs of the body. When this happens, this cancer affects the deeper tissue of the cervix and likely going to spread to other parts of the body such as the lungs,the bladder,liver,vagina and rectum.
Cervical cancer progresses slowly in the system through precancerous changes thereby providing the opportunities for early detection,treatment and prevention.
Women in their 20s and 30s are mostly diagnosed with precancerous changes in their cervix but the average age of women mostly diagnosed with cervical cancer are those in their mid 50s.
This difference in the age at which precancerous changes are most frequently diagnosed and the age at which cancer is diagnosed highlights the slow progression of this disease and the reason why it can be prevented if adequate steps are taken.
Causes of Cervical Cancer
Cervical cancer begins with abnormal changes in the cervical tissue. The risk of developing these abnormal changes is associated with infection with human papillomavirus (HPV). In addition, early sexual contact, multiple sexual partners, and taking oral contraceptives (birth control pills) increase the risk of cervical cancer because they lead to greater exposure to HPV.
Forms of HPV, a virus whose different types cause skin warts, genital warts, and other abnormal skin disorders, have been shown to lead to many of the changes in cervical cells that may eventually lead to cancer. Certain types of HPV have also been linked to cancers involving the vulva, vagina, penis, anus, tongue, and tonsils. Genetic material that comes from certain forms of HPV (high-risk subtypes) has been found in cervical tissues that show cancerous or precancerous changes.
In addition, women who have been diagnosed with HPV are more likely to develop a cervical cancer. Girls who begin sexual activity before age 16 or within a year of starting their menstrual periods are at high risk of developing cervical cancer.
Cigarette smoking is another risk factor for the development of cervical cancer. The chemicals in cigarette smoke interact with the cells of the cervix, causing precancerous changes that may over time progress to cancer. The risk of cervical cancer in cigarette smokers is two to five times that of the general population.
Oral contraceptives (“the pill”), especially if taken longer than five years, may increase the risk for cervical cancer because they reduce the use of condoms.
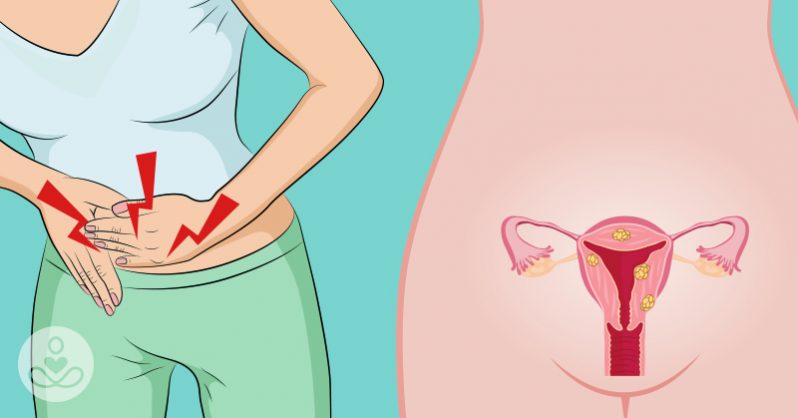
Symptoms Of Cervical Cancer
1.Pain, when the cancer is advanced
2.vaginal bleeding (other than during menstruation)
3.Abnormal vaginal discharge
4.Pelvic pain
5.Kidney failure due to a urinary tract or bowel obstruction, when
the cancer is advanced
When To Seek Medical Help
The range of conditions that can cause vaginal bleeding are diverse and may not be related to cancer of the cervix. They vary based on your age, fertility, and medical history.
Vaginal bleeding after menopause is never normal. If you have gone through menopause and have vaginal bleeding, see your health care provider as soon as possible.
Very heavy bleeding during your period or frequent bleeding between periods warrants evaluation by your health care provider.
Bleeding after intercourse, especially after vigorous sex, does occur in some women. If this occurs only occasionally, it is probably nothing to worry about. Evaluation by your health care provider is advisable, especially if the bleeding happens repeatedly.
If you have vaginal bleeding that is associated with weakness, feeling faint or light-headed, or actual fainting, go to a hospital emergency department for care.
Medical Treatment for Cervical Cancer
Treatment for precancerous lesions differs from that of invasive cervical cancer.
Choice of treatment for a precancerous lesion of the cervix depends on a number of factors, including whether the lesion is low or high grade, whether you want to have children in the future, your age and general health, and your preference and that of your health care provider.
If you have a low-grade lesion (CIN I, as detected by a Pap smear), you may not need further treatment, especially if the abnormal area was completely removed during biopsy. You should have regular Pap smears and pelvic exams, as scheduled by your doctor.
When a precancerous lesion requires treatment, LEEP conization, cold knife conization, cryosurgery (freezing), cauterization (burning, also called diathermy), or laser surgery may be used to destroy the abnormal area while minimizing damage to nearby healthy tissue.
Treatment for precancerous lesions may cause cramping or other pain, bleeding, or a watery vaginal discharge.
In some cases, you may choose to have a hysterectomy for precancerous changes, particularly if abnormal cells are found inside the opening of the cervix or you have severe or recurring dysplasia. This surgery is more likely to be done if you do not plan to have children in the future.
Diagnostic procedures, such as LEEP and cold knife conization, sometimes themselves may treat the cervical precancer, as well. Both involve taking tissue to evaluate. If the evaluation finds abnormal cells, but the cells do not extend into where the tissue was cut, only follow-up may be needed.
If there is uncertainty about whether all of the precancerous cells have been removed using LEEP or cold knife conization procedures, further treatments may be necessary.
Cryocautery may be used in some cases. In this procedure, a steel instrument is cooled to subzero temperatures by immersion in liquid nitrogen or a similar liquid. This ultracooled instrument is then applied to the surface of the cervix, freezing cells. They eventually die and are sloughed off, to be replaced by new cervical cells.
Tissue may also be removed by laser ablation. In this procedure, a laser beam is applied to either specific areas of cervical tissue or a whole layer of tissue at the surface of the cervix. The laser destroys these cells, leaving healthy cells in their place.